5 Diseases That Mimic Cushing's Syndrome

Cushing’s syndrome, a complex endocrine disorder, often presents a diagnostic challenge due to its diverse symptoms that can resemble other medical conditions. Here, we delve into five such diseases that share similarities with Cushing’s syndrome, exploring the key distinctions and the importance of accurate diagnosis and treatment.
Addison’s Disease
Addison’s disease, or primary adrenal insufficiency, is a rare endocrine disorder that occurs when the adrenal glands fail to produce sufficient cortisol and often aldosterone as well. This leads to a range of symptoms that can be mistaken for Cushing’s syndrome, including fatigue, weight loss, muscle weakness, and low blood pressure. However, unlike Cushing’s syndrome, individuals with Addison’s disease typically exhibit hyperpigmentation, especially in areas like the elbows, knees, knuckles, and mucous membranes.
A crucial differentiator between the two conditions is the underlying cause. While Cushing’s syndrome often results from excessive exposure to glucocorticoids, either through exogenous administration or endogenous overproduction, Addison’s disease is primarily caused by autoimmune destruction of the adrenal cortex.
Polycystic Ovary Syndrome (PCOS)
Polycystic ovary syndrome is a common endocrine disorder affecting women of reproductive age. It is characterized by a combination of hyperandrogenism, ovulatory dysfunction, and polycystic ovaries. Some symptoms of PCOS, such as weight gain, hirsutism, and irregular menstruation, can overlap with those of Cushing’s syndrome.
However, the key difference lies in the hormonal profile. In PCOS, elevated levels of androgens, such as testosterone, are a hallmark feature. In contrast, Cushing’s syndrome is associated with elevated levels of cortisol, often resulting from prolonged exposure to glucocorticoid hormones.
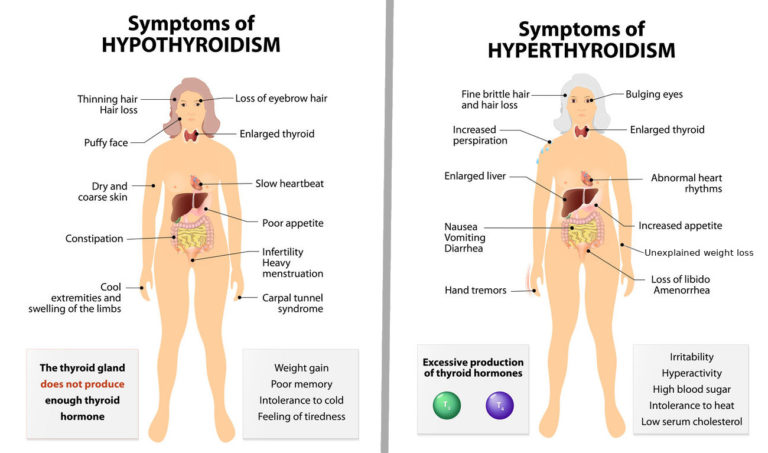
Hypothyroidism
Hypothyroidism, or underactive thyroid, occurs when the thyroid gland fails to produce sufficient thyroid hormones. This can lead to a range of symptoms, including fatigue, weight gain, cold intolerance, and constipation. While weight gain is a shared symptom with Cushing’s syndrome, the underlying mechanisms differ.
In hypothyroidism, the weight gain is typically accompanied by fluid retention and dry skin, whereas in Cushing’s syndrome, weight gain is often centralized, with increased fat deposition in the face, neck, and abdomen. Additionally, hypothyroidism is associated with low metabolic rate and reduced body temperature, which are not characteristic of Cushing’s syndrome.
Obesity
Obesity, a chronic condition characterized by excessive body fat, can present with symptoms that resemble Cushing’s syndrome, particularly in individuals with central obesity. These symptoms may include weight gain, central adiposity, fatigue, and mood disturbances.
However, obesity is a distinct condition from Cushing’s syndrome. While both can lead to similar physical changes, the underlying cause is different. Obesity is primarily a result of energy imbalance, where calorie intake exceeds expenditure over an extended period. In contrast, Cushing’s syndrome is caused by excess cortisol, either from exogenous sources or endogenous overproduction.
Type 2 Diabetes

Type 2 diabetes, a metabolic disorder characterized by insulin resistance and relative insulin deficiency, can also present with symptoms that mimic Cushing’s syndrome. These symptoms may include weight gain, particularly around the abdomen, increased appetite, and fatigue.
However, the key distinction lies in the hormonal profile and the underlying mechanisms. Type 2 diabetes is primarily driven by insulin resistance, where the body’s cells become less responsive to insulin, leading to elevated blood glucose levels. In contrast, Cushing’s syndrome is associated with elevated cortisol levels, which can lead to insulin resistance but is not the primary cause.
Accurate Diagnosis: The Key to Effective Treatment
Distinguishing Cushing’s syndrome from these mimickers is crucial for appropriate treatment. Misdiagnosis can lead to delays in managing the underlying condition and may result in unnecessary interventions or side effects.
For instance, in cases of suspected Cushing’s syndrome, a thorough evaluation of cortisol levels and their sources is essential. This may involve measuring cortisol levels at different times of the day, conducting stimulation and suppression tests, and imaging studies to identify potential sources of excess cortisol production.
Similarly, for conditions like Addison’s disease, PCOS, hypothyroidism, and obesity, accurate diagnosis is critical for managing symptoms and preventing complications. Each of these conditions requires a tailored approach to treatment, which may include hormone replacement therapy, lifestyle modifications, or medication to manage specific symptoms.
In conclusion, while Cushing’s syndrome can present a diagnostic challenge due to its diverse symptoms, understanding the key differences between it and other mimickers is essential for effective patient care. By recognizing these distinctions and employing appropriate diagnostic tools, healthcare providers can ensure timely and accurate diagnoses, leading to more targeted and successful treatment strategies.