Xerostomia: Unraveling the ICD-10 Mystery
Xerostomia, commonly known as dry mouth, is a condition that affects millions worldwide, yet its impact often remains hidden and under-discussed. This condition, characterized by a reduction in saliva production, can significantly impact an individual’s quality of life, leading to a range of oral health issues and discomfort. But what does the ICD-10 have to do with it? Let’s delve into the intricacies of this mysterious code and understand its role in diagnosing and treating xerostomia.
The ICD-10: Unlocking Diagnostic Doors

The International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) is a comprehensive system used by healthcare professionals worldwide to classify and code diseases, signs, symptoms, and other health-related conditions. It serves as a universal language, allowing medical professionals to communicate diagnoses and treatments accurately and efficiently. In the case of xerostomia, the ICD-10 provides a vital tool for healthcare providers to identify and address this often-overlooked condition.
Xerostomia: More Than Just Dryness

At its core, xerostomia is not merely a sensation of dryness in the mouth. It is a complex condition with a range of potential causes and consequences. Saliva plays a crucial role in maintaining oral health, aiding in digestion, and even protecting against infections. When saliva production decreases, it can lead to a host of issues, including:
- Oral Health Problems: Tooth decay, gum disease, and oral infections are more prevalent in individuals with xerostomia. Saliva helps neutralize acids produced by bacteria, and its absence can create an environment conducive to the growth of harmful microorganisms.
- Speech and Swallowing Difficulties: The lubricating properties of saliva are essential for smooth speech and swallowing. Reduced saliva can lead to discomfort, slurred speech, and difficulty swallowing, impacting an individual’s ability to communicate and eat.
- Taste Alteration: Saliva is integral to the sense of taste. Xerostomia can cause a change in taste perception, making food less enjoyable and potentially impacting an individual’s nutritional intake.
- Psychological Impact: The constant discomfort and oral health issues associated with xerostomia can lead to anxiety, depression, and a decreased quality of life.
Unraveling the ICD-10 Code
The ICD-10 code for xerostomia is K06.7, a specific designation that allows healthcare providers to identify and diagnose this condition accurately. This code is a powerful tool, enabling professionals to:
- Document and Track Xerostomia: By assigning the K06.7 code, healthcare providers can keep a record of xerostomia cases, allowing for better monitoring and management of the condition.
- Facilitate Research and Studies: The ICD-10 code provides a standardized way to collect and analyze data on xerostomia, aiding in research and the development of more effective treatments.
- Ensure Accurate Billing and Reimbursement: In healthcare systems that rely on coding for billing, the K06.7 code ensures that the diagnosis and treatment of xerostomia are appropriately recorded and reimbursed.
Understanding the Causes
Xerostomia can arise from a variety of factors, including:
- Medications: Many common medications, such as antihistamines, decongestants, and antidepressants, can cause dry mouth as a side effect.
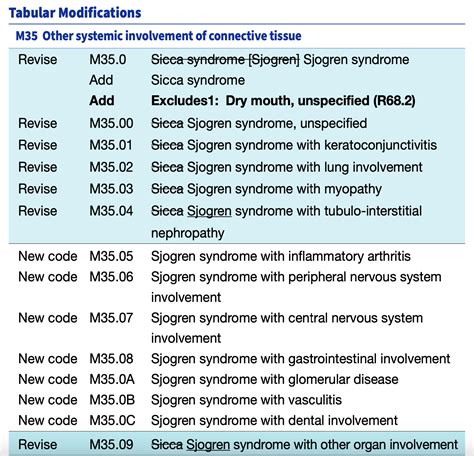
- Medical Conditions: Certain diseases and disorders, including Sjögren’s syndrome, diabetes, and Parkinson’s disease, are often associated with xerostomia.
- Radiation Therapy: Individuals undergoing head and neck radiation therapy may experience damage to the salivary glands, leading to reduced saliva production.
- Dehydration: Simple dehydration can also cause temporary xerostomia, emphasizing the importance of proper hydration for oral health.
Treatment and Management Strategies

While there is no single cure for xerostomia, various strategies can help manage the condition and alleviate its symptoms:
- Stimulate Saliva Production: Over-the-counter saliva substitutes and oral rinses can provide temporary relief. Sugar-free chewing gum or lozenges can also stimulate saliva flow.
- Medications: Prescription drugs, such as pilocarpine or cevimeline, can help stimulate saliva production in some cases.
- Oral Hygiene: Maintaining excellent oral hygiene is crucial. Regular brushing, flossing, and dental check-ups can help prevent tooth decay and gum disease.
- Hydration: Staying well-hydrated is essential. Drinking plenty of water and avoiding caffeine and alcohol, which can dehydrate the body, is recommended.
- Dietary Adjustments: Eating moist, soft foods and avoiding spicy or acidic foods can help manage xerostomia symptoms.
A Holistic Approach to Xerostomia Management
Effective management of xerostomia often requires a multidisciplinary approach, involving collaboration between healthcare professionals, including dentists, physicians, and speech therapists. This holistic approach ensures that the condition is addressed comprehensively, taking into account the various aspects of an individual’s health and well-being.
Conclusion: Empowering Patients and Professionals
Understanding the ICD-10 code for xerostomia is a crucial step in recognizing and addressing this often-overlooked condition. By using the K06.7 code, healthcare providers can ensure that xerostomia is accurately diagnosed and treated, leading to improved oral health and overall well-being for affected individuals. With a holistic approach and a range of management strategies, xerostomia can be effectively managed, allowing individuals to regain comfort and confidence in their daily lives.
What are some common symptoms of xerostomia?
+Common symptoms of xerostomia include a dry, sticky feeling in the mouth, frequent thirst, difficulty swallowing or speaking, altered taste perception, and increased susceptibility to oral infections and tooth decay.
Can xerostomia be prevented?
+While some causes of xerostomia, such as certain medications or medical conditions, may be unavoidable, maintaining good oral hygiene, staying hydrated, and regularly visiting the dentist can help reduce the risk and severity of xerostomia.
Are there any natural remedies for xerostomia?
+Some natural remedies, such as chewing sugar-free gum, sucking on ice chips, or using essential oils like peppermint or spearmint, may provide temporary relief. However, it’s essential to consult a healthcare professional for a comprehensive management plan.
How does xerostomia impact overall health?
+Xerostomia can have a significant impact on overall health, affecting nutrition, speech, and even mental well-being. It increases the risk of oral infections and tooth decay, which, if left untreated, can lead to more serious health complications.



