Mastering the Art of Soap Note in Physical Therapy

In the world of physical therapy, the SOAP note stands as a cornerstone for documenting patient care, treatment progress, and outcomes. SOAP, an acronym for Subjective, Objective, Assessment, and Plan, provides a structured approach to record keeping, ensuring that therapists can efficiently capture and communicate vital patient information. This article delves into the intricacies of creating effective SOAP notes, offering insights and strategies to enhance their value in physical therapy practice.
Unraveling the SOAP Note Structure
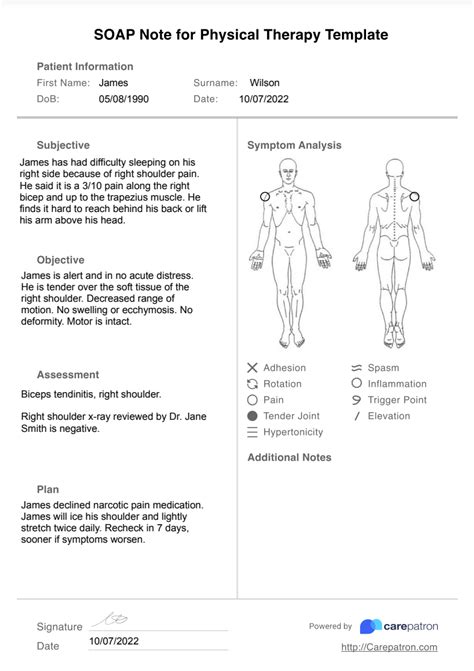
The SOAP note format is a systematic approach to documenting patient encounters, offering a comprehensive view of the patient’s journey through physical therapy. Each component plays a unique role in capturing the patient’s experience and progress.
Subjective (S): The Patient’s Perspective
The subjective section of the SOAP note is the patient’s voice. It captures the patient’s description of their symptoms, concerns, and experiences. This includes the nature and location of pain, the onset and duration of symptoms, and any aggravating or alleviating factors. For instance, a patient might describe their pain as a “sharp, shooting pain in the lower back that worsens with prolonged sitting.”
| Subjective Element | Description |
|---|---|
| Chief Complaint | A concise statement of the primary reason for seeking therapy. |
| Symptoms | A detailed account of physical sensations and functional limitations. |
| Medical History | Relevant past and current medical conditions, surgeries, and medications. |

Objective (O): The Therapist’s Observations
The objective section is where the physical therapist’s expertise comes to the forefront. It includes the therapist’s observations, measurements, and findings from physical examinations and tests. This data provides an evidence-based perspective on the patient’s condition.
| Objective Element | Description |
|---|---|
| Physical Examination | Details of range of motion, strength, and neurological tests. |
| Measurements | Quantitative data such as weight, height, BMI, and vital signs. |
| Imaging and Lab Results | Interpretation of X-rays, MRIs, and blood work relevant to the condition. |
Assessment (A): Synthesizing Information
The assessment section is where the therapist integrates the subjective and objective data to formulate a diagnosis or problem list. It involves identifying the root causes of the patient’s symptoms and establishing clear goals for treatment.
| Assessment Element | Description |
|---|---|
| Diagnosis | A clear statement of the patient's primary condition. |
| Problem List | A comprehensive list of issues requiring attention. |
| Goals | Short-term and long-term objectives for treatment. |
Plan (P): Charting the Course
The plan section outlines the therapist’s strategy for addressing the patient’s needs. It includes the types of interventions, frequency of treatments, and expected outcomes. This section guides the patient’s care and provides a roadmap for the therapy process.
| Plan Element | Description |
|---|---|
| Interventions | Specific treatments, exercises, and modalities to be used. |
| Frequency and Duration | How often and for how long each intervention will be applied. |
| Expected Outcomes | Clear, measurable goals for the patient's progress. |
Maximizing the Value of SOAP Notes

SOAP notes are more than just a documentation requirement; they are a powerful tool for enhancing patient care and outcomes. Here’s how therapists can optimize their SOAP notes to achieve the best results.
Consistency and Detail
Consistency is key in SOAP note writing. Therapists should maintain a uniform format for each component, ensuring that all relevant information is captured. Attention to detail is vital, as it provides a comprehensive view of the patient’s condition and progress.
Incorporating Technology
Physical therapy practice management software often includes features that streamline SOAP note creation. These tools can automate data entry, provide templates, and offer secure storage, ensuring efficient and compliant record keeping.
Collaborative Care
SOAP notes are not just for the therapist’s eyes. They are a communication tool that can enhance collaboration among healthcare professionals. Sharing relevant information with other providers can lead to better-coordinated care and improved patient outcomes.
Patient Engagement
Involving patients in the SOAP note process can increase their understanding of their condition and treatment. Therapists can discuss the note with patients, ensuring they are informed and active participants in their care journey.
Future Implications and Innovations
As physical therapy practice evolves, so too will the methods of documentation. The future of SOAP notes may involve more integration with electronic health records (EHRs) and advanced analytics. This could lead to more efficient data capture and analysis, providing therapists with deeper insights into patient care.
Additionally, the use of natural language processing and artificial intelligence could revolutionize SOAP note creation, allowing for more automated documentation and potentially improving the accuracy and speed of record keeping.
What is the primary purpose of a SOAP note in physical therapy?
+SOAP notes serve as a structured framework for documenting patient encounters, ensuring a comprehensive record of the patient’s symptoms, the therapist’s observations, and the treatment plan. They provide a clear, organized view of the patient’s journey through physical therapy, aiding in effective communication and decision-making.
How often should a SOAP note be updated?
+SOAP notes should be updated after each significant patient encounter or whenever there is a change in the patient’s condition, treatment plan, or progress. Regular updates ensure that the note remains an accurate and up-to-date reflection of the patient’s therapy journey.
Can SOAP notes be shared with patients or other healthcare providers?
+Absolutely. SOAP notes are a valuable tool for communication and collaboration. Sharing them with patients can enhance their understanding of their condition and treatment, while sharing with other healthcare providers can lead to more coordinated, effective care.



