5 Key Steps for Effective Physical Exam SOAP Notes

1. Subjective Assessment: Unraveling the Patient's Story

The subjective assessment forms the foundation of any physical exam SOAP note. It is here that the patient’s narrative takes center stage, offering a wealth of information that guides the diagnostic process. To craft an effective subjective assessment, consider these key elements:
Chief Complaint: Begin by capturing the patient’s primary concern or reason for seeking medical attention. This concise statement sets the tone for the entire assessment, providing a snapshot of the patient’s current health status.
History of Present Illness: Dive deeper into the patient’s narrative, exploring the timeline of their symptoms, any associated factors, and the impact on their daily life. This section requires active listening and empathy, as patients often provide crucial clues that can lead to accurate diagnoses.
Past Medical History: Documenting the patient’s medical journey is essential. Note any previous diagnoses, surgeries, or treatments, as this information can significantly influence the current assessment and treatment plan.
Social and Family History: The patient’s social and familial context can offer valuable insights. Factors such as occupation, lifestyle, and family medical history may impact their health and treatment outcomes.
Medications and Allergies: A comprehensive list of current medications and known allergies is vital. This information ensures the patient’s safety and guides the prescription of appropriate treatments.
2. Objective Findings: A Scientific Approach
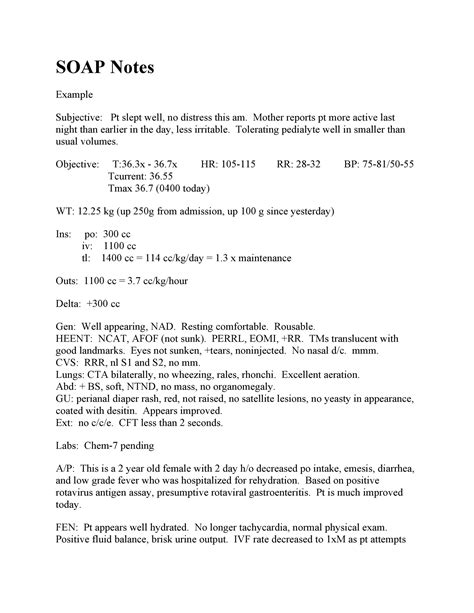
While the subjective assessment relies on the patient’s narrative, the objective findings section takes a scientific approach, focusing on observable data and measurable results. This section is where the physical exam comes to life, providing concrete evidence to support the patient’s story. Here’s how to approach it:
Vital Signs: Begin by documenting the patient’s vital signs, including blood pressure, heart rate, respiratory rate, and temperature. These baseline measurements are crucial indicators of the patient’s overall health and can reveal underlying conditions.
Physical Examination: This is the heart of the physical exam. Conduct a thorough examination, noting any abnormalities or findings in a systematic manner. Use clear and concise language to describe observations, such as “mild edema in the lower extremities” or “crackles auscultated in the lung bases.”
Laboratory and Diagnostic Tests: If applicable, include the results of any relevant laboratory tests or diagnostic imaging. These findings provide additional objective data to support the assessment and guide treatment decisions.
Measurements and Calculations: Depending on the specialty, measurements such as height, weight, body mass index (BMI), or specific calculations like Glasgow Coma Scale (GCS) scores may be necessary. Ensure these are accurately recorded.
3. Assessment and Plan: Interpreting the Evidence
The assessment and plan section is where the subjective and objective findings come together to form a cohesive diagnosis and treatment strategy. This section requires critical thinking and clinical expertise:
Differential Diagnosis: Present a list of potential diagnoses based on the gathered evidence. Rank them in order of likelihood, considering the patient’s unique circumstances.
Most Likely Diagnosis: Select the diagnosis that best fits the patient’s presentation and explain the reasoning behind this choice.
Treatment Plan: Outline the proposed treatment strategy, including medications, therapies, or interventions. Provide clear instructions and educate the patient on the expected outcomes and potential risks.
Follow-up and Monitoring: Determine the appropriate follow-up schedule and any necessary monitoring or testing to ensure the patient’s progress is on track.
4. Documentation Standards: Ensuring Consistency and Compliance
Maintaining consistent and compliant documentation standards is essential for effective communication and legal protection. Here are some key considerations:
Timeliness: Ensure that SOAP notes are completed promptly, preferably within 24 hours of the physical exam. Timely documentation reduces the risk of critical information being overlooked or forgotten.
Legibility and Clarity: Use a clear and legible handwriting style or, preferably, electronic documentation systems. Ensure that all entries are easily readable and free from errors or abbreviations that may cause confusion.
Privacy and Confidentiality: Protect patient privacy by adhering to HIPAA guidelines. Only include necessary information and ensure secure storage and transmission of electronic records.
Consistency: Maintain a consistent format and structure throughout your SOAP notes. This consistency aids in quick information retrieval and ensures a standardized approach across healthcare providers.
5. Continuous Improvement: Learning from Every Encounter

Physical exam SOAP notes are not merely administrative tasks; they are opportunities for continuous learning and improvement. Reflect on each encounter to enhance your clinical skills:
Review and Learn: Regularly review your SOAP notes to identify areas for improvement. Seek feedback from colleagues and mentors to refine your assessment and documentation skills.
Stay Current: Keep abreast of the latest medical advancements and best practices. Attend conferences, read journals, and engage in continuous professional development to ensure your assessments and plans remain up-to-date.
Collaborate and Communicate: Foster a culture of open communication within your healthcare team. Share insights and learn from the experiences of others to enhance your diagnostic and treatment strategies.
What is the primary purpose of SOAP notes in physical exams?
+SOAP notes serve as a structured framework for documenting physical exam findings, ensuring a comprehensive and organized record of the patient's assessment and treatment plan. They facilitate effective communication between healthcare providers and provide a reference for future care.
<div class="faq-item">
<div class="faq-question">
<h3>How often should SOAP notes be updated during a patient's treatment journey?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>SOAP notes should ideally be updated after each significant encounter with the patient, such as follow-up visits, changes in treatment plans, or the occurrence of new symptoms. Regular updates ensure that the documentation remains current and reflects the patient's evolving health status.</p>
</div>
</div>
<div class="faq-item">
<div class="faq-question">
<h3>Are there any legal considerations when creating SOAP notes?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Absolutely. Healthcare providers must adhere to legal and ethical standards when creating SOAP notes. This includes maintaining patient confidentiality, ensuring accuracy and completeness of records, and following guidelines such as HIPAA to protect patient privacy.</p>
</div>
</div>
<div class="faq-item">
<div class="faq-question">
<h3>How can healthcare providers improve their subjective assessment skills?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Improving subjective assessment skills requires active listening, empathy, and a deep understanding of the patient's perspective. Healthcare providers can enhance these skills through ongoing training, mentorship, and a commitment to patient-centered care.</p>
</div>
</div>
<div class="faq-item">
<div class="faq-question">
<h3>What are some common challenges in creating effective SOAP notes, and how can they be overcome?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Common challenges include time constraints, maintaining legibility, and ensuring comprehensive documentation. To overcome these, prioritize tasks, utilize electronic health record systems, and collaborate with colleagues to streamline the documentation process while maintaining accuracy and completeness.</p>
</div>
</div>
</div>
In the intricate world of healthcare documentation, physical exam SOAP notes are a powerful tool. By following these five steps and embracing the art and science of effective documentation, healthcare providers can unlock the full potential of their physical exam assessments, ultimately leading to improved patient care and outcomes.



