Brain Scans: Uncovering OCD's Secrets
Unraveling the Complex World of OCD: Insights from Brain Scans
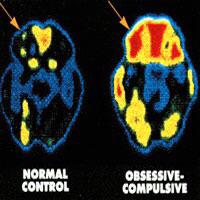
Brain scans have revolutionized our understanding of various mental health conditions, and Obsessive-Compulsive Disorder (OCD) is no exception. By peering into the intricate workings of the brain, researchers are shedding light on the secrets of this complex disorder. Let’s delve into the fascinating insights revealed by these advanced imaging techniques.
Understanding OCD Through Brain Imaging

OCD is a mental health disorder characterized by intrusive thoughts, obsessions, and repetitive behaviors or compulsions. While the exact causes remain elusive, brain scans offer a unique window into the underlying neural processes. Here’s a glimpse into what scientists have discovered:
The Brain’s Fear Circuitry
One of the key findings from brain scans is the activation of the brain’s fear circuitry in individuals with OCD. This circuitry, which includes regions such as the amygdala and the anterior cingulate cortex, is involved in processing fear and threat responses. Researchers have observed heightened activity in these areas during OCD-related tasks, suggesting a potential link between OCD symptoms and an overactive fear response.
For instance, a study using functional magnetic resonance imaging (fMRI) found increased connectivity between the amygdala and other brain regions in OCD patients compared to healthy controls. This hyperconnectivity may contribute to the heightened anxiety and fear experienced by individuals with OCD.
Dysfunction in the Frontal Lobes
The frontal lobes, responsible for executive functions like decision-making and impulse control, also play a crucial role in OCD. Brain scans have revealed abnormalities in this region, particularly in the orbitofrontal cortex and the anterior cingulate cortex.
These abnormalities can manifest as reduced gray matter volume or altered functional connectivity. For example, a study published in the Journal of Psychiatric Research found reduced gray matter volume in the orbitofrontal cortex of OCD patients, suggesting a potential structural basis for the impaired decision-making often seen in this disorder.
Overactive Reward System
Surprisingly, brain scans have also revealed an overactive reward system in individuals with OCD. This finding challenges the traditional view of OCD as solely driven by fear and anxiety. Researchers have observed increased activity in brain regions associated with reward processing, such as the striatum and the nucleus accumbens, during OCD-related tasks.
This overactivity may explain why compulsive behaviors, which provide temporary relief from anxiety, can become highly rewarding and reinforce the OCD cycle. Understanding this aspect of OCD opens up new avenues for treatment, targeting both the fear and reward components of the disorder.
Unraveling the Neurochemical Landscape

Brain scans not only provide structural and functional insights but also offer a glimpse into the neurochemical landscape of OCD. By measuring neurotransmitter levels and activity, researchers are gaining a deeper understanding of the biochemical imbalances underlying this disorder.
Serotonin and OCD
Serotonin, a neurotransmitter associated with mood and anxiety regulation, has long been implicated in OCD. Brain scans using positron emission tomography (PET) have revealed reduced serotonin transporter availability in the brains of OCD patients. This finding suggests that impaired serotonin transmission may contribute to the development and maintenance of OCD symptoms.
Additionally, studies have shown that selective serotonin reuptake inhibitors (SSRIs), a class of antidepressants, can effectively reduce OCD symptoms. This further supports the role of serotonin in OCD and highlights the potential of targeted pharmacological interventions.
Beyond Serotonin: Dopamine and Glutamate
While serotonin has been a primary focus, brain scans have also shed light on the involvement of other neurotransmitters. Dopamine, often associated with reward and motivation, has been implicated in OCD, particularly in relation to the rewarding nature of compulsive behaviors.
Furthermore, emerging evidence suggests a role for glutamate, a neurotransmitter involved in learning and memory, in OCD. Studies have shown altered glutamate levels in the brains of OCD patients, particularly in regions such as the anterior cingulate cortex and the striatum. This finding opens up new avenues for exploring glutamate-targeted treatments for OCD.
Personalized Treatment Approaches
The insights gained from brain scans are not only enhancing our understanding of OCD but also paving the way for personalized treatment approaches. By identifying specific neural signatures associated with different subtypes of OCD, researchers can tailor interventions to individual needs.
For example, brain scans have revealed distinct patterns of brain activity in OCD patients with primarily compulsive symptoms compared to those with primarily obsessional symptoms. This knowledge allows clinicians to develop targeted cognitive-behavioral therapies, medication regimens, or even explore the potential of brain stimulation techniques like transcranial magnetic stimulation (TMS) for specific OCD subtypes.
Conclusion: A Glimpse into the Future
Brain scans are providing a remarkable glimpse into the complex world of OCD, offering insights that were previously unimaginable. As research in this field continues to advance, we can expect even more refined understanding of the neural underpinnings of OCD.
By combining brain imaging techniques with other innovative approaches, such as genetic studies and real-time monitoring of neural activity, researchers are poised to unlock the secrets of OCD and develop more effective treatments. The future of OCD research is indeed an exciting journey, one that holds the promise of improved quality of life for those affected by this challenging disorder.
FAQ

How do brain scans help in understanding OCD better than traditional methods?
+Brain scans provide a direct glimpse into the neural activity and structure of the brain, offering insights that traditional methods like self-reports or behavioral observations cannot capture. By visualizing the brain in action, researchers can identify specific neural signatures associated with OCD, leading to a more nuanced understanding of the disorder.
Can brain scans predict the severity of OCD symptoms in an individual?
+While brain scans have provided valuable insights into the neural correlates of OCD, predicting the severity of symptoms in an individual based solely on brain scans is still an evolving area of research. However, ongoing studies are exploring the potential of using brain imaging biomarkers to predict treatment response and symptom severity, which could revolutionize personalized medicine for OCD.
Are there any ethical considerations when using brain scans for OCD research?
+Absolutely. The use of brain scans for OCD research raises important ethical considerations, particularly around privacy, informed consent, and potential stigma. Researchers must adhere to strict ethical guidelines to ensure the protection of participants’ rights and maintain confidentiality. Additionally, careful interpretation of brain scan data is crucial to avoid potential misinterpretations or misuse.
How do brain scans contribute to the development of new treatments for OCD?
+Brain scans play a crucial role in guiding the development of new treatments for OCD. By identifying specific neural abnormalities associated with different subtypes of OCD, researchers can design targeted interventions, whether it’s cognitive-behavioral therapies, medication regimens, or even novel approaches like brain stimulation techniques. This personalized medicine approach holds great promise for improving treatment outcomes.



