Mesenchymal Stem Cells: Unlocking Regenerative Power
Mesenchymal stem cells (MSCs) have emerged as a groundbreaking force in the field of regenerative medicine, offering unprecedented potential to heal and repair damaged tissues and organs. These remarkable cells, which can differentiate into various cell types, are at the forefront of cutting-edge research and therapeutic strategies. With their unique abilities, MSCs are unlocking new avenues for treating a wide range of conditions, from cardiovascular diseases to neurological disorders, and even providing hope for previously untreatable injuries.
The Origin and Nature of MSCs
Mesenchymal stem cells are a type of adult stem cell found in various tissues throughout the body, including bone marrow, adipose tissue, and the umbilical cord. Unlike embryonic stem cells, which are pluripotent and can differentiate into any cell type, MSCs are multipotent, capable of differentiating into a limited number of cell lineages. This characteristic, while seemingly restrictive, actually offers a targeted approach to regenerative medicine, allowing scientists to focus on specific cell types needed for particular treatments.
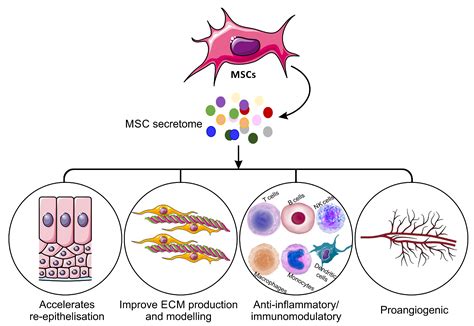
One of the key advantages of MSCs is their ability to migrate to injured or diseased areas within the body. This homing property is essential for their therapeutic potential, as it ensures that these stem cells can reach the sites where they are most needed. Once at the injury site, MSCs can initiate a range of regenerative processes, including secreting growth factors and cytokines, promoting angiogenesis (the formation of new blood vessels), and even directly differentiating into specific cell types to replace damaged tissue.
Therapeutic Applications of MSCs

The versatility and therapeutic potential of MSCs have led to their exploration in a vast array of medical conditions. Here’s a glimpse into some of the most promising applications:
Cardiovascular Disease
MSCs have shown particular promise in the treatment of cardiovascular diseases, including heart attacks and myocardial infarction. When introduced into the affected area, these stem cells can differentiate into cardiomyocytes, the specialized muscle cells of the heart, potentially restoring damaged heart tissue and improving cardiac function. Clinical trials have demonstrated encouraging results, with MSCs showing the ability to reduce infarct size and improve heart function in patients with myocardial infarction.
Neurological Disorders
The brain and spinal cord, due to their limited regenerative capacity, are particularly challenging areas for therapeutic interventions. However, MSCs have shown the potential to revolutionize the treatment of neurological disorders. In conditions such as Parkinson’s disease, multiple sclerosis, and spinal cord injuries, MSCs can differentiate into neural cells, promoting tissue repair and potentially restoring lost neurological functions. Additionally, their immunomodulatory properties can help reduce inflammation and prevent further damage in these conditions.
Orthopedic Injuries and Diseases
MSCs have a long history of use in orthopedic medicine, particularly in the treatment of bone and cartilage injuries. Their ability to differentiate into osteoblasts (bone cells) and chondrocytes (cartilage cells) makes them ideal for repairing fractures, treating osteoarthritis, and even regenerating bone and cartilage in complex orthopedic injuries. Furthermore, their anti-inflammatory properties can help manage the chronic inflammation often associated with orthopedic conditions.
Autoimmune Diseases
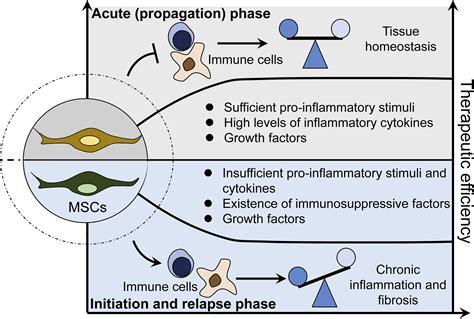
The immunomodulatory properties of MSCs make them a potential game-changer in the treatment of autoimmune diseases, where the body’s immune system mistakenly attacks its own tissues. MSCs can regulate the immune response, reducing inflammation and promoting immune tolerance. This has led to their exploration in conditions such as rheumatoid arthritis, lupus, and multiple sclerosis, with clinical trials showing promising results in terms of symptom reduction and improved quality of life.
Challenges and Future Prospects
While the potential of MSCs is undeniable, there are challenges that must be addressed to fully harness their power. One of the primary concerns is ensuring the safety and efficacy of MSC-based therapies. As with any stem cell treatment, there is a risk of adverse events, including immune reactions and the potential for MSCs to form tumors. Rigorous clinical trials and further research are essential to understand and mitigate these risks.
Another challenge lies in optimizing the methods for isolating, expanding, and delivering MSCs. Currently, the process of isolating MSCs from adult tissues can be time-consuming and costly. Researchers are exploring new methods, such as the use of MSCs derived from induced pluripotent stem cells, which could provide a more accessible and consistent source of these therapeutic cells.
Looking ahead, the future of MSC-based therapies appears promising. With continued research and innovation, we can expect to see MSCs playing an increasingly important role in the treatment of a wide range of conditions. The ability to harness the body’s own regenerative power holds the potential to transform the landscape of medicine, offering new hope and improved quality of life for patients worldwide.
What are the main sources of mesenchymal stem cells used in therapeutic applications?
+The primary sources of MSCs for therapeutic use include bone marrow, adipose tissue, and the umbilical cord. Each source has its advantages and challenges, with bone marrow MSCs being the most widely studied and utilized, but also the most invasive to harvest. Adipose-derived MSCs are easier to obtain, while umbilical cord-derived MSCs offer an ethically non-controversial source but require careful banking and processing.
How do MSCs differentiate into specific cell types?
+MSCs possess the unique ability to differentiate into various cell types based on environmental cues and specific growth factors. This process, known as differentiation, is carefully regulated by the cells’ genetic machinery. By exposing MSCs to specific conditions and growth factors, researchers can guide them to become the desired cell type, such as osteoblasts, chondrocytes, or neural cells.
Are there any ethical concerns surrounding the use of MSCs in medicine?
+Ethical concerns primarily surround the source of MSCs. While adult MSCs derived from bone marrow, adipose tissue, or the umbilical cord are generally considered ethically acceptable, there are debates surrounding the use of embryonic stem cells to generate MSCs. However, with the advent of induced pluripotent stem cells, which can be derived from adult cells, many of these ethical concerns are being addressed.
What are the potential risks of MSC-based therapies?
+Like any medical treatment, MSC-based therapies carry potential risks. These include immune reactions, where the body rejects the transplanted MSCs, and the possibility of tumor formation. Additionally, there are concerns about the long-term effects of MSCs, as their behavior and fate after transplantation are still not fully understood. However, rigorous clinical trials and ongoing research aim to mitigate these risks.
How close are we to seeing MSC-based therapies become mainstream medical treatments?
+MSCs have already made their way into clinical practice, with a number of therapies being approved or in advanced stages of clinical trials. However, the field is still evolving, and many therapies are considered experimental. As research continues to advance and more data is gathered, we can expect to see MSC-based treatments become more widely available and accepted within the medical community.



