5 Essential Tips for Treating Horner's Syndrome

Horner’s syndrome is a rare neurological condition that affects the nerves responsible for controlling various functions in the face and eyes. While it can be a challenging condition to manage, there are effective strategies to alleviate symptoms and improve the quality of life for those affected. In this article, we delve into five essential tips that can make a significant difference in treating Horner’s syndrome.
Understanding the Condition
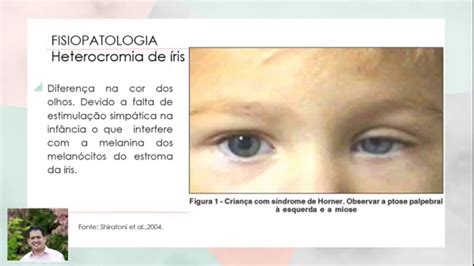
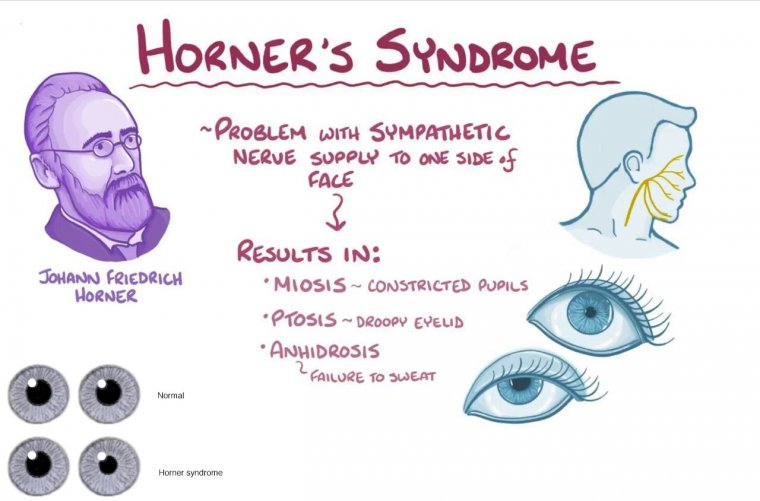
Horner’s syndrome, also known as oculosympathetic palsy, arises from a disruption in the sympathetic nervous system, which regulates involuntary body functions. This disruption often occurs due to an underlying issue in the neck or upper spinal cord. The condition is characterized by a unique set of symptoms, including:
- Drooping of the upper eyelid (ptosis)
- Constriction of the pupil (miosis)
- Reduced sweating on one side of the face (anhidrosis)
- Slight elevation of the lower eyelid
- Redness and flushing of the affected eye
These symptoms can vary in severity and may not always be noticeable to the individual. However, recognizing and addressing Horner’s syndrome promptly is crucial for effective management.
Tip 1: Identify and Treat the Underlying Cause

The first step in managing Horner’s syndrome is to identify and address the underlying cause. Since the condition is often a secondary effect of another medical issue, treating the primary problem is essential. Common causes include:
- Neck or upper spinal cord injuries
- Tumors in the neck or chest region
- Stroke or transient ischemic attack (TIA)
- Carotid artery dissection
- Cluster headaches or migraines
Work closely with your healthcare team to diagnose the underlying condition accurately. Treatment approaches may vary depending on the cause, ranging from surgical interventions to medication management.
Tip 2: Medication Management
In some cases, medications can help alleviate specific symptoms of Horner’s syndrome. For instance, if the condition is caused by a migraine or cluster headache, preventative medications or acute treatments can provide relief. Additionally, medications to manage any associated pain or discomfort can significantly improve the patient’s quality of life.
Tip 3: Symptomatic Relief Techniques
While addressing the underlying cause is crucial, managing the symptoms of Horner’s syndrome is equally important for the patient’s comfort and daily functioning. Here are some practical strategies:
- Eyelid Management: Drooping eyelids can affect vision and cause discomfort. Eyelid crutches or specialized glasses with an attached crutch can help support the eyelid and improve vision.
- Sun Protection: The affected eye may be more sensitive to light, so wearing sunglasses with UV protection is recommended.
- Moisturization: Anhidrosis can lead to dry skin on the affected side of the face. Using a good moisturizer can help alleviate dryness and prevent skin irritation.
- Regular Eye Examinations: Regular visits to an ophthalmologist are essential to monitor any changes in eye health and ensure timely intervention if needed.
Tip 4: Physical Therapy and Rehabilitation
Physical therapy plays a vital role in managing the long-term effects of Horner’s syndrome, especially if the condition is caused by a neurological injury or trauma. A tailored physical therapy program can:
- Improve muscle strength and coordination
- Enhance balance and stability
- Reduce pain and stiffness
- Promote overall physical well-being
Working with a qualified physical therapist can significantly improve the patient’s functional abilities and overall quality of life.
Tip 5: Emotional Support and Coping Strategies
Living with a chronic condition like Horner’s syndrome can be emotionally challenging. It’s essential to address the psychological impact and provide support for the patient’s well-being. Consider the following:
- Education: Understanding the condition and its implications can empower patients to take an active role in their treatment.
- Support Groups: Connecting with others who share similar experiences can provide valuable emotional support and practical advice.
- Psychological Counseling: Talking to a mental health professional can help patients cope with the emotional and social aspects of living with Horner’s syndrome.
- Mind-Body Practices: Techniques like meditation, yoga, or deep breathing exercises can reduce stress and improve overall well-being.
Conclusion
While Horner’s syndrome can present unique challenges, a comprehensive and multidisciplinary approach to treatment can make a significant difference in managing the condition. By addressing the underlying cause, implementing practical strategies, and providing emotional support, individuals with Horner’s syndrome can lead fulfilling and comfortable lives. Remember, each person’s journey is unique, and finding the right combination of treatments is key to successful management.
What are the common causes of Horner's syndrome in children?
+In children, Horner's syndrome can be caused by various factors, including birth trauma, congenital conditions, or tumors. Prompt diagnosis and treatment are crucial to prevent long-term complications.
Can Horner's syndrome be reversed?
+The reversibility of Horner's syndrome depends on the underlying cause. If the condition is caused by a treatable issue, such as a reversible neck injury, recovery is possible. However, in some cases, the symptoms may be permanent.
Are there any alternative therapies for managing Horner's syndrome symptoms?
+While traditional medical treatments are the primary approach, some individuals find relief through complementary therapies like acupuncture or herbal remedies. However, these should be discussed with a healthcare provider.
How often should patients with Horner's syndrome undergo eye examinations?
+Regular eye examinations are recommended every 6-12 months to monitor eye health and detect any potential complications. The frequency may vary depending on the individual's specific condition and symptoms.
Remember, this article provides a general overview, and individual experiences may vary. Always consult with healthcare professionals for personalized advice and treatment plans.



