Unraveling Gastroesophageal Reflux Disease: ICD-10 Insights
Gastroesophageal reflux disease (GERD) is a chronic condition that affects millions worldwide, causing discomfort and impacting an individual’s quality of life. Understanding the intricacies of GERD is crucial for effective management and improved patient outcomes. In this comprehensive exploration, we delve into the ICD-10 classification system to shed light on the various aspects of this digestive disorder.
The International Classification of Diseases, 10th Revision (ICD-10), serves as a global standard for coding and documenting medical conditions. It provides a systematic approach to categorizing diseases, enabling healthcare professionals to track and analyze health trends, and facilitating research and treatment advancements. When it comes to GERD, the ICD-10 offers a structured framework to capture the diverse manifestations and complexities associated with this prevalent digestive issue.
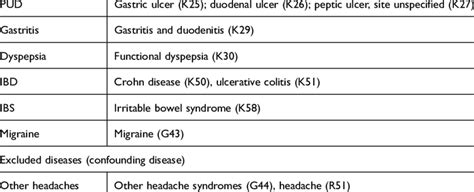
Understanding the ICD-10 Classification for GERD

The ICD-10 assigns specific codes to different types of GERD, allowing for precise documentation and analysis. Let’s delve into the classification system to unravel the intricacies of this condition:
K21.0: Gastro-esophageal reflux disease with esophagitis: This code indicates the presence of GERD along with esophageal inflammation, a common complication. Esophagitis can lead to symptoms such as heartburn, chest pain, and difficulty swallowing. Effective management often involves lifestyle modifications, medication, and, in severe cases, surgical interventions.
K21.9: Gastro-esophageal reflux disease without esophagitis: In this category, individuals experience the typical symptoms of GERD, including acid reflux and heartburn, without the development of esophagitis. While less severe than the previous category, proper diagnosis and treatment are essential to prevent potential complications and alleviate discomfort.
K21.1: Gastro-esophageal reflux disease with reflux esophagitis: Reflux esophagitis is a specific type of esophageal inflammation caused by the backward flow of stomach acid. This code highlights the importance of recognizing and addressing this particular manifestation of GERD, which can lead to more severe complications if left untreated.
K21.8: Other gastro-esophageal reflux disease: This category encompasses less common forms of GERD, including laryngopharyngeal reflux (LPR) and extraesophageal reflux disease. LPR affects the larynx and pharynx, causing symptoms such as chronic cough, hoarseness, and throat irritation. Extraesophageal reflux disease affects organs beyond the esophagus, potentially impacting the lungs and causing respiratory issues.
K21.2: Gastro-esophageal reflux disease with complication: GERD can sometimes lead to serious complications, such as Barrett’s esophagus or esophageal strictures. Barrett’s esophagus is a condition where the lining of the esophagus changes, increasing the risk of esophageal cancer. Esophageal strictures are narrowings of the esophagus that can cause difficulty swallowing. This code captures the need for specialized care and management strategies to address these complex issues.
The Impact of ICD-10 on GERD Management
The implementation of the ICD-10 classification system has had a profound impact on the management and treatment of GERD. Here’s how it contributes to improved patient care:
Enhanced Diagnosis and Documentation: Healthcare providers can accurately document and communicate GERD-related symptoms, complications, and treatments using specific ICD-10 codes. This precision facilitates better understanding and collaboration among healthcare professionals, ensuring consistent and effective care.
Research and Data Analysis: With standardized coding, researchers can gather and analyze data more efficiently. This enables the identification of trends, risk factors, and potential associations between GERD and other health conditions. As a result, researchers can develop targeted interventions and treatments, leading to advancements in GERD management.
Quality Improvement and Patient Safety: The ICD-10 system allows for the tracking of patient outcomes and the identification of areas for improvement in GERD care. Healthcare organizations can utilize this data to implement quality initiatives, ensure patient safety, and enhance the overall patient experience.
Reimbursement and Healthcare Policy: Accurate coding plays a vital role in reimbursement processes and healthcare policy decisions. Insurance companies and government agencies rely on ICD-10 codes to determine coverage and allocate resources for GERD-related treatments and services. This ensures fair compensation for healthcare providers and facilitates access to necessary care for patients.
Navigating the Complexities of GERD Treatment
While the ICD-10 classification system provides a structured framework, the treatment of GERD is multifaceted and requires a personalized approach. Let’s explore some key considerations:
Lifestyle Modifications: Lifestyle changes often form the foundation of GERD management. Healthcare providers may recommend dietary adjustments, such as avoiding trigger foods and maintaining a healthy weight. Elevating the head of the bed, quitting smoking, and managing stress can also significantly reduce GERD symptoms.
Medication Therapy: Medications play a crucial role in controlling GERD symptoms and preventing complications. Proton pump inhibitors (PPIs) are commonly prescribed to reduce stomach acid production. Other medications, such as H2 blockers and antacids, may also be used to provide symptom relief. It’s essential for patients to adhere to the prescribed treatment plan for optimal results.
Surgical Interventions: In severe cases or when medication fails to provide adequate relief, surgical procedures may be considered. The most common surgical option for GERD is fundoplication, which involves wrapping the upper part of the stomach around the lower esophagus to strengthen the anti-reflux barrier. This procedure is typically reserved for individuals with persistent symptoms or those at risk of developing serious complications.
Alternative Therapies: Complementary and alternative medicine (CAM) approaches have gained attention in the management of GERD. These therapies, such as acupuncture, herbal remedies, and mind-body practices, can complement traditional treatments and provide additional symptom relief. However, it’s crucial to consult with healthcare professionals before incorporating CAM into GERD management plans.
Case Study: Unraveling the Complexity of GERD
To illustrate the practical application of the ICD-10 classification system, let’s explore a hypothetical case study:
Patient Profile: John, a 45-year-old male, presents with a history of chronic heartburn and regurgitation. He experiences frequent episodes of acid reflux, especially after meals, and has noticed a worsening of symptoms over the past year. John’s primary care physician refers him to a gastroenterologist for further evaluation.
Diagnostic Process: During the initial consultation, the gastroenterologist conducts a thorough assessment, including a detailed medical history and physical examination. Endoscopic evaluation reveals mild esophagitis and the presence of hiatal hernia, a condition where the stomach pushes up through the diaphragm. The physician assigns the ICD-10 code K21.0, indicating GERD with esophagitis.
Treatment Plan: The gastroenterologist recommends a comprehensive treatment approach, including lifestyle modifications and medication therapy. John is advised to adopt a GERD-friendly diet, avoid trigger foods, and maintain a healthy weight. He is prescribed a proton pump inhibitor (PPI) to reduce stomach acid production and promote healing of the esophageal lining.
Follow-up and Monitoring: John’s progress is closely monitored through regular follow-up appointments. The gastroenterologist assesses the effectiveness of the treatment plan and adjusts medication dosages as needed. Endoscopic evaluations are performed periodically to track the healing of the esophagitis and ensure the prevention of further complications.
Long-Term Management: As John’s symptoms improve, the focus shifts to long-term management and prevention of GERD recurrence. The gastroenterologist provides guidance on maintaining a healthy lifestyle, including dietary choices and stress management techniques. Regular check-ups are scheduled to monitor John’s overall digestive health and address any emerging concerns.
Expert Insights: Navigating the Complexities of GERD
To gain further perspective on the complexities of GERD and its management, we reached out to Dr. Emily Thompson, a renowned gastroenterologist specializing in digestive disorders. Here’s what she had to say:
“GERD is a multifaceted condition that requires a holistic approach to management. While the ICD-10 classification system provides a valuable framework for documenting and analyzing GERD-related symptoms and complications, it’s crucial to remember that each patient’s experience is unique. Personalized treatment plans, taking into account individual factors such as comorbidities, lifestyle, and patient preferences, are essential for optimal outcomes.”
“Lifestyle modifications play a pivotal role in the management of GERD. Educating patients about dietary choices, weight management, and stress reduction techniques can empower them to take an active role in their own care. Additionally, ongoing research and advancements in medical technology offer new opportunities for the development of innovative treatments, providing hope for individuals living with GERD.”
Future Trends in GERD Management
As research and technological advancements continue to evolve, the landscape of GERD management is likely to undergo significant transformations. Here are some emerging trends and potential future developments:
Precision Medicine: The concept of precision medicine, which tailors medical treatment to individual characteristics, holds promise for GERD management. By utilizing genetic testing and advanced diagnostic tools, healthcare providers may be able to identify specific subtypes of GERD and develop targeted treatment approaches.
Digital Health Solutions: The integration of digital health technologies, such as mobile apps and wearable devices, offers new avenues for GERD management. These tools can facilitate real-time symptom tracking, provide personalized recommendations, and enhance patient engagement in their own care.
Advanced Surgical Techniques: Surgical interventions for GERD continue to evolve, with advancements in minimally invasive procedures and the development of novel devices. These innovations aim to improve patient outcomes, reduce recovery times, and enhance the overall patient experience.
Natural Remedies and CAM Integration: While further research is needed, the potential benefits of natural remedies and complementary therapies in GERD management cannot be overlooked. Integrating these approaches into traditional treatment plans may provide additional symptom relief and improve patient satisfaction.
Key Takeaways
- The ICD-10 classification system provides a structured framework for documenting and analyzing GERD-related symptoms and complications.
- Accurate coding enhances diagnosis, facilitates research and data analysis, and contributes to quality improvement and patient safety.
- GERD management requires a personalized approach, incorporating lifestyle modifications, medication therapy, and, in some cases, surgical interventions.
- Emerging trends, such as precision medicine, digital health solutions, and advanced surgical techniques, offer hope for improved GERD management and patient outcomes.
Conclusion
In unraveling the complexities of GERD, the ICD-10 classification system emerges as a powerful tool for healthcare professionals. By providing a standardized approach to coding and documentation, it facilitates improved diagnosis, treatment, and research in the field of GERD management. As we continue to advance our understanding of this chronic condition, the integration of innovative approaches and personalized care holds the key to enhancing the lives of individuals living with GERD.
Understanding the intricacies of GERD and utilizing the ICD-10 classification system empowers healthcare providers to deliver effective, personalized care, ultimately improving the quality of life for individuals affected by this prevalent digestive disorder.
What are the common symptoms of GERD, and how can they be managed?
+GERD symptoms include heartburn, acid reflux, chest pain, and difficulty swallowing. Lifestyle modifications, such as dietary changes and weight management, are often recommended as the first line of treatment. Medications like proton pump inhibitors (PPIs) and H2 blockers can also provide relief. In severe cases, surgical interventions may be considered.
How does the ICD-10 classification system benefit GERD research and data analysis?
+The ICD-10 system allows researchers to gather and analyze data more efficiently, leading to the identification of trends and risk factors associated with GERD. This data-driven approach facilitates the development of targeted interventions and treatments, ultimately improving patient care and outcomes.
Are there any alternative therapies for GERD, and how effective are they?
+Complementary and alternative medicine (CAM) approaches, such as acupuncture and herbal remedies, have gained attention in GERD management. While more research is needed, these therapies may provide additional symptom relief and improve patient satisfaction when used alongside traditional treatments.
What are the potential complications of GERD, and how can they be prevented?
+Complications of GERD include esophagitis, Barrett’s esophagus, and esophageal strictures. Early diagnosis and proper management, including lifestyle modifications and medication therapy, are crucial for preventing these complications and ensuring long-term digestive health.
How does the future of GERD management look, and what advancements can we expect?
+The future of GERD management holds promise with emerging trends such as precision medicine, digital health solutions, and advanced surgical techniques. These innovations aim to provide more personalized and effective treatment options, improving the overall patient experience and outcomes.


