Cytomegalovirus: Essential Isolation Precautions
Cytomegalovirus (CMV) is a common virus that can cause serious health complications, especially in individuals with weakened immune systems. Healthcare facilities and medical professionals must implement stringent isolation precautions to prevent the spread of CMV and protect vulnerable patients. This comprehensive guide outlines the essential measures required for effective CMV isolation, ensuring the safety and well-being of patients and healthcare workers.
Understanding Cytomegalovirus

Cytomegalovirus, a member of the herpesvirus family, is prevalent worldwide. While most healthy individuals with robust immune systems can effectively fight off CMV without noticeable symptoms, it can pose significant risks to specific populations. Pregnant women, newborns, and individuals with compromised immune systems, such as organ transplant recipients and those with HIV/AIDS, are particularly vulnerable to CMV-related complications.
CMV Transmission and High-Risk Settings

CMV transmission occurs primarily through bodily fluids, including saliva, urine, blood, and breast milk. Close personal contact, such as kissing or sharing utensils, can facilitate the spread of the virus. In healthcare settings, CMV can be transmitted through contaminated medical equipment or via healthcare workers who have the virus but exhibit no symptoms.
Hospitals and healthcare facilities that cater to immunocompromised patients are at higher risk of CMV transmission. These settings include bone marrow transplant units, solid organ transplant wards, and specialized care units for patients with HIV/AIDS.
Essential Isolation Precautions for CMV
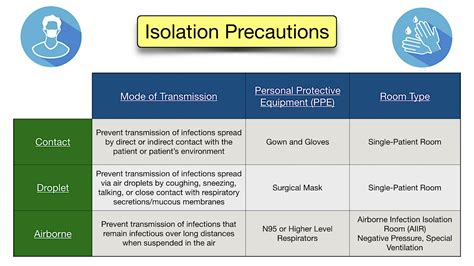
To prevent CMV transmission and protect vulnerable patients, healthcare facilities must adhere to stringent isolation precautions. These measures are designed to create a safe environment, minimizing the risk of CMV exposure and subsequent infection.
Implementing Standard Precautions
Standard precautions are fundamental infection control measures that apply to all patients, regardless of their suspected or confirmed infection status. These precautions form the foundation of safe patient care and are essential in preventing the spread of CMV and other pathogens.
- Hand Hygiene: Healthcare workers must practice rigorous hand hygiene before and after patient contact, as well as before and after any invasive procedure. Hand hygiene involves either washing hands with soap and water or using an alcohol-based hand rub.
- Personal Protective Equipment (PPE): PPE, such as gloves, gowns, masks, and eye protection, should be worn when providing care to any patient. PPE creates a barrier between the healthcare worker and the patient, reducing the risk of CMV transmission.
- Respiratory Hygiene: Respiratory hygiene measures, including coughing etiquette and the use of masks, are crucial in preventing the spread of respiratory pathogens, including CMV.
- Safe Injection Practices: Adherence to safe injection practices, such as using sterile equipment for each patient and disposing of sharps properly, is essential in preventing CMV transmission through contaminated medical equipment.
Contact Precautions for CMV
In addition to standard precautions, healthcare facilities should implement contact precautions when caring for patients with confirmed or suspected CMV infection. Contact precautions are designed to prevent the transmission of pathogens through direct or indirect contact with the patient or their environment.
- Gown and Glove Use: Healthcare workers should wear gowns and gloves when entering the room of a patient with confirmed or suspected CMV infection. Gowns and gloves should be removed and disposed of properly before leaving the patient’s room.
- Patient Room Assignment: Patients with confirmed or suspected CMV infection should be placed in single-patient rooms, if available. If a single-patient room is not feasible, cohorting (grouping) patients with the same infection status can be considered.
- Dedicated Equipment: Whenever possible, dedicated medical equipment should be used for the care of CMV-infected patients. This equipment should not be used for other patients to prevent cross-contamination.
- Environmental Cleaning: Rigorous environmental cleaning and disinfection practices should be implemented in the patient’s room. High-touch surfaces, such as bedrails, doorknobs, and medical equipment, should be cleaned frequently using appropriate disinfectants.
Droplet Precautions for CMV
CMV can be transmitted through respiratory droplets, making droplet precautions essential when caring for patients with confirmed or suspected CMV infection. These precautions are designed to prevent the spread of pathogens through respiratory secretions.
- Mask Use: Healthcare workers should wear a surgical mask when entering the room of a patient with confirmed or suspected CMV infection. The mask should cover the nose and mouth and be worn consistently during patient care.
- Patient Cough Etiquette: Patients with confirmed or suspected CMV infection should be educated on proper cough etiquette. They should cover their mouth and nose with a tissue when coughing or sneezing and dispose of the tissue properly. If a tissue is not available, they should cough or sneeze into their elbow, not their hands.
- Airborne Precautions: In rare cases, CMV can be transmitted through airborne droplets. When caring for patients with confirmed or suspected CMV infection involving the lungs, healthcare facilities should implement airborne precautions, including the use of N95 respirators for healthcare workers and negative pressure rooms for patient isolation.
Educating Healthcare Workers and Patients
Effective isolation precautions for CMV rely on the knowledge and adherence of healthcare workers and patients. Education and training programs should be implemented to ensure that all staff members understand the importance of infection control measures and the specific precautions required for CMV.
Patients and their families should also be educated on CMV transmission and the importance of adhering to isolation precautions. Clear and concise communication can help patients understand the reasons behind certain restrictions and encourage their cooperation.
Continuous Monitoring and Adaptation

CMV isolation precautions should be regularly monitored and adapted based on the latest scientific evidence and best practices. Healthcare facilities should have robust infection control policies and procedures in place, with designated personnel responsible for overseeing and updating these measures.
Frequently Asked Questions (FAQs)
What is the incubation period for CMV infection?
+The incubation period for CMV infection can vary but typically ranges from 4 to 6 weeks. However, it's important to note that some individuals may experience a longer incubation period, especially if their immune system is compromised.
Are there any specific symptoms of CMV infection that healthcare workers should look out for?
+CMV infection can present with a range of symptoms, including fever, fatigue, muscle aches, and swollen lymph nodes. In immunocompromised individuals, CMV can cause more severe symptoms, such as pneumonia, hepatitis, and neurological complications. Healthcare workers should be vigilant for these signs and symptoms and consider CMV as a potential cause.
How long do healthcare workers need to follow isolation precautions for a CMV-infected patient?
+The duration of isolation precautions depends on the clinical status of the patient and the specific guidelines of the healthcare facility. In general, isolation precautions should be maintained until the patient is no longer considered infectious. This may be determined by the resolution of symptoms, negative CMV tests, or a predetermined period based on the patient's condition.
Can CMV be transmitted through blood transfusions or organ transplants?
+Yes, CMV can be transmitted through blood transfusions and organ transplants. Healthcare facilities should have strict screening protocols in place to identify CMV-positive donors and take appropriate precautions to minimize the risk of transmission to recipients.
Are there any effective treatments for CMV infection?
+While there is no cure for CMV infection, antiviral medications can be used to manage the infection and prevent complications. The choice of medication and duration of treatment depend on the patient's clinical condition and the severity of the infection. Healthcare providers should carefully monitor patients receiving antiviral therapy for CMV.
Conclusion
Cytomegalovirus is a potentially serious pathogen that requires vigilant infection control measures, particularly in healthcare settings. By implementing and adhering to essential isolation precautions, healthcare facilities can create a safer environment for patients and healthcare workers, reducing the risk of CMV transmission and subsequent complications. Continuous education, monitoring, and adaptation of isolation protocols are crucial in ensuring the highest standards of patient care and infection control.



