Unraveling the Chest X-ray Mystery

The Intricate Art of Chest X-ray Interpretation

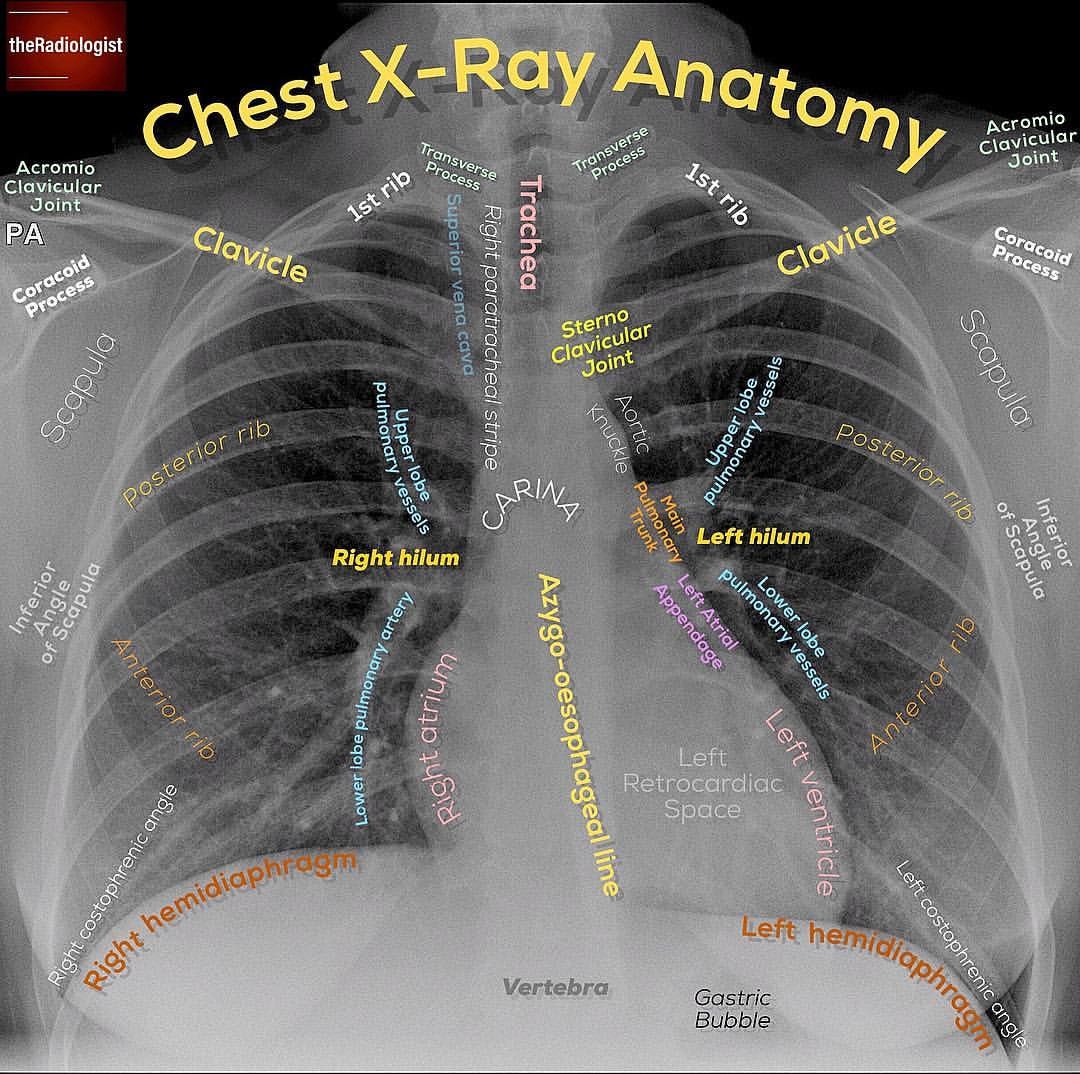
Delving into the world of chest radiography, we embark on a journey that uncovers the subtle intricacies hidden within these images. While X-rays may appear simple at first glance, they are intricate maps that, when deciphered, reveal a wealth of information about the human chest cavity. This process is an art, a scientific pursuit, and a critical skill for healthcare professionals.
Chest X-rays are a cornerstone of diagnostic medicine, offering a non-invasive window into the thoracic region. They can provide a wealth of information, from identifying fractures and foreign objects to revealing the presence of diseases such as pneumonia, tuberculosis, or even cancer. However, interpreting these images is a complex task that requires a keen eye, extensive training, and a deep understanding of the human anatomy.
Interpreting chest X-rays is akin to reading a complex novel. Each image contains layers of information, and the key is to unravel the story it tells.
Dr. Emma Anderson, RadiologistUnderstanding the Basics

Before we delve into the intricacies of interpretation, let’s establish some fundamental concepts.
Anatomy of a Chest X-ray
A standard chest X-ray consists of two views: the posteroanterior (PA) view and the lateral view. The PA view is taken with the X-ray beam directed from the back to the front of the patient, while the lateral view captures the side profile. These two views provide complementary information, offering a comprehensive view of the thoracic cavity.
Pros of PA View
- Better visualization of the heart and mediastinum.
- Clearer view of the diaphragm and lower lung fields.
- More accurate assessment of rib fractures and other bony structures.
Cons of PA View
- Can be challenging to obtain in patients who are critically ill or immobile.
- Requires patient cooperation for accurate positioning.
Common Findings on Chest X-rays
Chest X-rays can reveal a wide array of findings, ranging from normal variations to life-threatening conditions. Some common findings include:
Pneumonia: This infection of the lung tissue can cause consolidation, an increased opacity seen on X-rays, often with air bronchograms.
Pleural Effusion: An accumulation of fluid in the pleural space, visible as a dense opacity along the chest wall.
Pneumothorax: The presence of air in the pleural cavity, often resulting from a traumatic event or lung disease.
Pulmonary Edema: Caused by fluid accumulation in the lungs, leading to a hazy, ground-glass appearance on X-rays.
Fractures: X-rays can detect fractures of the ribs, clavicle, or scapula, which appear as discontinuities in the bone outline.
The Art of Interpretation
Interpreting chest X-rays is a multi-step process that requires a systematic approach. Here’s a step-by-step guide to unraveling the mystery:
Step 1: Assess Image Quality
Before delving into the interpretation, ensure the image quality is adequate. Poor image quality can obscure important findings. Check for:
Adequate exposure: The image should not be too light or too dark, obscuring details.
Proper positioning: Ensure the patient is correctly positioned, with no rotation or tilt that could distort the image.
Absence of artifacts: Artifacts, such as EKG leads or external objects, can obscure important areas of the chest.
Step 2: Global Assessment
Start with a global assessment of the X-ray. Look for overall symmetry and any gross abnormalities. Consider the following:
Cardiac Silhouette: Is it enlarged or shifted? An enlarged cardiac silhouette can indicate heart failure or pericardial effusion.
Diaphragm: Check for elevation or flattening. Elevated hemidiaphragms can indicate subdiaphragmatic air or fluid.
Mediastinum: Evaluate for any deviation or widening, which can suggest mediastinal pathology.
Lung Fields: Look for consolidation, opacities, or infiltrates that could indicate pneumonia or other lung diseases.
Step 3: Detail Analysis
Now, zoom in on specific areas of the chest to look for finer details.
Bone Structures: Assess the ribs, clavicle, and scapula for fractures or abnormalities.
Lungs: Look for nodules, masses, or cavitations that could indicate cancer or infectious processes.
Pleura: Check for pleural thickening, calcifications, or effusions.
Mediastinum: Evaluate the mediastinal contours and structures for any abnormalities.
Step 4: Correlate with Clinical Information
Interpretation of chest X-rays is not done in isolation. Correlate the findings with the patient’s clinical presentation, laboratory results, and other imaging studies to reach a comprehensive diagnosis.
Consider the patient’s symptoms, such as chest pain, shortness of breath, or fever.
Look for clues in laboratory results, such as elevated white blood cell count suggesting infection.
Compare with previous X-rays to assess for any changes or progression of disease.
Expert Perspective: Unraveling the Complex
Chest X-ray interpretation is a complex skill that requires years of training and experience. It's a delicate balance of art and science, where each image tells a unique story. With practice, one learns to recognize patterns and abnormalities, but the key is always to approach each X-ray with a fresh eye and an open mind.
Dr. William Parker, RadiologistNavigating the Challenges
Interpreting chest X-rays is not without its challenges. Some common pitfalls and obstacles include:
Overreading: Interpreting normal variations as pathological findings.
Underreading: Missing subtle abnormalities due to a lack of experience or attention to detail.
Technical Limitations: Poor image quality or patient positioning can obscure important findings.
Interobserver Variability: Different radiologists may interpret the same X-ray differently, highlighting the need for consistent training and protocols.
Conclusion: A Vital Diagnostic Tool
Chest X-rays are a vital diagnostic tool in the field of medicine, offering a non-invasive window into the thoracic cavity. While interpreting these images is a complex skill, with proper training and experience, healthcare professionals can unlock the mysteries hidden within these radiographic maps.
Remember, the key to successful interpretation lies in a systematic approach, attention to detail, and a thorough understanding of the patient’s clinical context.
How long does it take to become proficient in chest X-ray interpretation?
+Proficiency in chest X-ray interpretation typically requires several years of training and experience. Radiology residents undergo extensive training during their residency, which can last 4-5 years. However, even after residency, ongoing learning and practice are crucial to maintain and enhance interpretation skills.
<div class="faq-item">
<div class="faq-question">
<h3>Can chest X-rays miss certain conditions?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Yes, while chest X-rays are a valuable diagnostic tool, they can sometimes miss certain conditions. For example, small lung nodules or early-stage cancer may not be visible on X-rays, especially if they are located in areas obscured by other structures. This is why multiple imaging modalities and clinical correlation are often necessary for a comprehensive diagnosis.</p>
</div>
</div>
<div class="faq-item">
<div class="faq-question">
<h3>What are some common errors in chest X-ray interpretation?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Common errors in chest X-ray interpretation include overreading normal variations as pathologies and underreading subtle abnormalities. Other errors may arise from poor image quality, improper patient positioning, or a lack of clinical correlation. Consistent training, quality control measures, and interobserver consensus can help mitigate these errors.</p>
</div>
</div>
<div class="faq-item">
<div class="faq-question">
<h3>How often should chest X-rays be performed for routine screening?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Routine chest X-ray screening is generally not recommended for healthy individuals without specific risk factors or symptoms. However, for those with certain conditions, such as lung cancer or tuberculosis, periodic screening may be advised. The frequency of screening depends on individual risk factors and should be discussed with a healthcare provider.</p>
</div>
</div>
<div class="faq-item">
<div class="faq-question">
<h3>Are there any alternatives to chest X-rays for diagnosing thoracic conditions?</h3>
<span class="faq-toggle">+</span>
</div>
<div class="faq-answer">
<p>Yes, several alternative imaging modalities can be used to diagnose thoracic conditions. These include computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans. Each modality has its strengths and weaknesses, and the choice depends on the specific clinical scenario and the suspected condition.</p>
</div>
</div>
</div>